A New Hormone Study Hits Headlines and Backlash Begins Again
By Sarah A LoBisco, ND
The past few weeks, I’ve been filling my brain with reading research studies on Hormone Replacement Therapy (HT) and re-listening to my trainings from the Institute of Functional Medicine. It’s definitely a very broad topic and functional medicine is not about making a protocol practitioner. True, protocols can make a lot of money by marketing the latest trend, but as a Naturopathic Doctor, I want to know the root cause of any symptom or disease manifestation.
If someone is considering HT, I desire to dig deeper on why someone’s hormones are unbalanced to begin with. I would also want to explore with them how to support their wellness on all levels. I don’t agree with the use of anything, including hormones, as a band aid approach to symptoms. For example, it may be popular to use progesterone for mood issues or estrogen for hot flashes, but without addressing and supporting the cause of deregulation, more symptoms could manifest. Furthermore, hormonal interventions are powerful, and I stand firmly behind upholding the Hippocrates Oath of “First Do No Harm.”
Last week, I promised I would provide some answers that I’ve come to conclude regarding various topics in hormone replacement (HT) use and its risks. To do this effectively, I wanted to give you some important background on why the answers aren’t so clear cut and explain why, in my opinion, any recommendation needs to be customized and individualized for safely using external sources of hormones.
Why Are Hormones Such a Hot Topic
Since the Women’s Health Initiative (WHI) halted clinical trials of HT in 2002 and 2004, there has been a controversy amongst experts in the use and safety of HT in women. Their preliminary results indicated an increased risk of breast cancer and heart disease with estrogen plus progesterone and estrogen alone therapy, respectively. This understandably made many physicians reconsider recommending its use for bone, heart, or hormonal health.
Within the past few years, my colleagues and I have been getting whip-lashed by a whirlwind of studies on HT hitting our heads. These studies were trying to extrapolate when a woman would benefit or be harmed through this external manipulation of their biochemistry by these powerful hormones. Often, these studies were reporting conflicting recommendations from reanalysis of the original clinical trials or new trials recommended competing factors for outcomes to consider!
To make matters even more clouded, POOF- a new money market also began. Media personalities began touting benefits or promising amazing results with using hormones. Studies were put in books that, if one didn’t have a full knowledge of the literature, seemed convincing, but cautions were often under reported.
So.. as a physician who doesn’t just prescribe blindly, that’s a lot of cerebral stress and makes the way for a lot of studying to keep up with the celebrities and misinformation. Well, conflict and disagreement are definitely, news…hence hormones are hot topic!
As you recall, in the spring I posted an update on hormonal health and the use of hormones. Now, a new meta-analysis is bringing attention back to the “estrogen controversy.”
This recent comparison study included women aged 50-59 years who had hysterectomies and received placebo in the randomized trials of WHI.
- The authors used a derived formula to relate the excess mortality among this population compared to the entire population of comparable women in the United States.
- The study accounted for the decline in estrogen use observed between 2002 and 2011 due to the Women’s Health Initiative (WHI) scare.
The authors concluded that between 18?601 and as many as 91?610 postmenopausal women died prematurely because of the avoidance of estrogen therapy (ET).
According to Yale News:
Women and their doctors became frightened of the dangers of post-menopausal hormones. But according to Sarrel and his colleagues, this was a report about women with a uterus, who took pills that combined estrogen and a progestin. Women who have a uterus must take a second hormone (a progestin) to avoid a risk of uterine cancer. But these results did not apply to women with no uterus who use estrogen-only therapy.
The Backlash Hits!
Dr. Katz, one of the researchers defended his findings on the Huffington Post:
… Clearly, the intent from the start was to generate data in this huge clinical trial with real-world application. Clearly, the intent from the start was to extrapolate the WHI findings to all other women like those in the trial. That’s exactly what we did, merely adding the rigor of a cautious mathematical model.
Hormone Use: What to Consider when Considering??!!
So, what to do??
Here’s what I feel is important when a woman or man is considering supplementing with hormones:
1. First of all, let’s remember whenever a secondary analysis of an original trial is reevaluated and extrapolated (as above); a very delicate statistical dance with even more stringent restrictions must be considered. This is in order to ensure that a result is truly from an intervention and not from chance, placebo effects, or other confounders.
The original JAMA trial of 2011, in which the above study extrapolated from was based on a comparison study of women with very important caveats:
- They all had a hysterectomy; therefore, they were in very different hormonal state then women who still had ovaries or a uterus.
- It was within a specific age population of 50-79 years (see the age factor in lab measurements of my Saratoga.com blog).
- The mean follow up was 5.9 years
Take home point one: Consider your own unique hormonal characteristics and wellness history when assessing risks and benefits of hormone replacement.
2. Just because a symptom disappears by the application of a medicine or supplement, doesn’t necessarily mean the risk factors, underlying issues, or predisposition to a connected disease has been addressed!
In other words, just because the use of progesterone or estrogen led to decreased hot flashes, it doesn’t mean that hormones are balanced. In fact, supplementing hormones without considering all the factors that influence them can create more imbalances down the road.
For example:
-women who use progesterone alone and who have low estrogen levels could feed forward cortisol production and blood sugar deregulation
–testosterone use for libido could convert to more estrogen production. For some women, this could lead to increasing estrogen cancer risks, blood sugar issues, irritability, and aggression
–women who use hormones and have compromised detoxification or genetic issues with hormonal breakdown in their livers and could increase their production of disease promoting inflammatory estrogen byproducts
–progesterone does have effects on breast tissue long term (even if it helps your bones and hot flashes right now)
Take home point two: Consider risk factors that will be affected when considering hormone replacement.
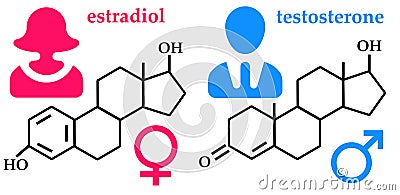
3. Every time one hormone shifts, other hormones are affected. This means that anytime a hormone is used simply for a symptom without considering a strong foundation of stress support, biotransformation of hormones, clearance of environmental chemicals, or blood sugar regulations, the symptom and side effect shuffle begin.
Hormones exist more in a soup, rather than a biochemical pathway. Feedback and regulation to the brain, nervous system, circulation, immune system, digestive track, and detoxification are all affected by any hormone!
For example:
-increased estrogens increase proteins and clotting factors in the liver, part of the explanation for heart risks in hormone replacement trials
-stress effects insulin which effects estrogen use in the body and resultant balance with progesterone
-all hormones effect mood
Take home point three: Consider the risks on other organ systems when considering hormone replacement.
4. Method of delivery:
Estrogen taken by mouth has a very different effect on liver metabolism of hormones then estrogen delivery in other methods.
Take home point four: Consider the method of delivery
I consider a woman’s lifestyle, history, ability to detoxify and modulate estrogen exposures, and genetic risk factors in a hormonal discussion consult.
In fact, I even try to consider factors one might not think of. For example, there is evidence of elevated insulin-like-growth factor in tall men and women and could be something to consider. One controlled factor study of an analysis of 20, 928 postmenopausal women concluded:
They found that for every 4-inch change in height, there was a 13 percent increase in risk for developing any type of cancer. The cancers most strongly associated with height were cancers of the kidney, rectum, thyroid and blood. Risk for those cancers increased by 23 to 29 percent for every 4-inch increase in height.
This is why hormones are a good example of the founding principles of BREAKFREE Medicine-that everything and every kind of “treatment” needs to be individualized.
What about blood tests?
Now, what about labs for testing hormones?
Click here to read about lab testing in a continuation of What to Consider with Hormone Replacement.
For other natural solutions for hormonal balance, read here.
References:
Department of Health and Human Services, The National Institutes of Health (NIH), National Heart, Lung, and Blood Institute (NHLBI). WHI Background and Overview. http://www.nhlbi.nih.gov/whi/background.htm. Accessed August 5, 2013.
Brown, E. Study Upholds Breast Cancer Mortality For Hormone Replacement. Los Angeles Times (latimes.com). March 30, 2013.
National Cancer Institute. Oral Contraceptives and Cancer Risk. NCI. 4/22/13 accessed. http://www.cancer.gov/cancertopics/factsheet/Risk/oral-contraceptives
National Cancer Institute. Hormone Replacement Therapy and Breast Cancer Relapse. NCI.
National Cancer Institute. NCI. Menopausal Hormone Therapy and Cancer. http://www.cancer.gov/cancertopics/factsheet/Risk/menopausal-hormones
LaCrox, AZ et al. Health outcomes after stopping conjugated equine estrogens among postmenopausal women with prior hysterectomy: a randomized controlled trial. JAMA. 2011 Apr 6;305(13):1305-14. doi: 10.1001/jama.2011.382. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3656722/
Sarrel PM, Njike VY, Vinante V, Katz DL. The Mortality Toll of Estrogen Avoidance: An Analysis of Excess Deaths Among Hysterectomized Women Aged 50 to 59 Years (abstract). Am J Public Health. 2013 Jul 18. doi:10.2105/AJPH.2013.301295. PMID: 23865654
Katz, D. Estrogen and Evidence. HuffingtonPost.com. July 23, 2013. http://www.huffingtonpost.com/david-katz-md/estrogen-meopause_b_3639915.html
Weir, W. Yale: Avoiding Estrogen Led To Thousands Of Needless Deaths: Hormone Could Have Saved Lives Of Women With Hysterectomies, Study Finds. Courant.com. July 18, 2013. http://articles.courant.com/2013-07-18/health/hc-estrogen-therapy-0719-20130717_1_estrogen-only-therapy-hormone-therapy-yale-study
Peart, K. For women with hysterectomies, estrogen may be a lifesaver after all. Yale News. (online). July 18m 2013. http://news.yale.edu/2013/07/18/women-hysterectomies-estrogen-may-be-lifesaver-after-all
Parker-Pope, T. Cancer Risk Increases With Height. New York Times. July 25, 2013. http://well.blogs.nytimes.com/2013/07/25/cancer-risk-increases-with-height/?partner=rss&emc=rss&_r=1
Mercola, J. Estrogen Could Have Prevented Almost 50,000 Deaths. Mercola.com.August 05, 2013.http://articles.mercola.com/sites/articles/archive/2013/08/05/hormone-replacement-therapy.aspx?e_cid=20130805_DNL_art_1&utm_source=dnl&utm_medium=email&utm_content=art1&utm_campaign=20130805
Lohrn, A. Global Consensus Statement on Menopausal Hormone Therapy. Endocrine.org. (The Endocrine Society). https://www.endocrine.org/news-room/current-press-releases/global-consensus-statement-on-menopausal-hormone-therapy
North American Menopause Society. The 2012 hormone therapy position statement of: The North American Menopause Society (abstract). Menopause [online]. 2012 Mar;19(3):257-71. doi: 10.1097/gme.0b013e31824b970a.
The American College of Obstetricians and Gynecologists. Hormone therapy and heart disease. Committee Opinion No. 565. American College of Obstetricians and Gynecologists. Obstet Gynecol 2013;121:1407–10. http://www.acog.org/Resources%20And%20Publications/Committee%20Opinions/Committee%20on%20Gynecologic%20Practice/Hormone%20Therapy%20and%20Heart%20Disease.aspx
Announcements and News:

1. Do you like what you read here?
I post updates on news that may not make my blogs on my Facebook page.
Join us and share your thoughts! I would love to “meet” you!
My new BREAKFREE MEDICINE Facebook Page

2. What is Estrogen Dominance?
Hormonal replacement can lead to Estrogen Dominance which can create a variety of imbalances in the body.
3. The Winners are Announced!
Thank you Katherine and Mary for your belly rolling hormonal tales!
It was awesome to meet you at the amazing performance of Menopause the Musical!
4. Phone Consultation Update:
Due to increasing travel, writing, training, presentations, an increased national clientele, and research, I will be transitioning to asking more of my clients to reap the benefits of phone consultations!
5. Book of the Month: Mind Over Medicine by Lissa Rankin, MD
Dr. Rankin reveals her discovery that the health care she had been taught to practice was missing something crucial: a recognition of the body’s innate ability to self-repair and an appreciation for how we can control these self-healing mechanisms with the power of the mind. She empowers you to make your own Diagnosis, write your own Prescription, and create a clear action plan designed to help you make your body ripe for miracles.
My blog on Dr. Lissa Rankin’s Health Health Care Now Website
6. Visit me on Dr. Oz’s Sharecare